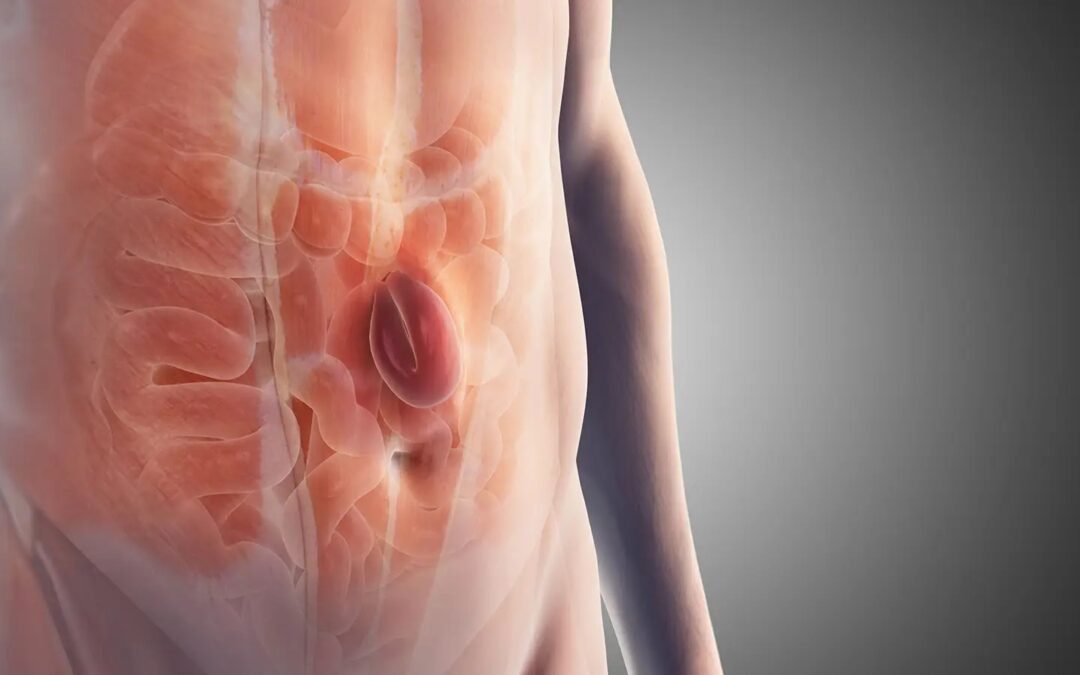
In most cases, hernias are successfully treated with surgery. However, there are instances where hernias fail, leading to complications or recurrence. But why do hernia repairs fail? What exactly causes a hernia to fail? and How can these failures be prevented?
Why Do Hernia Repairs Fail? Factors to Consider
Hernia repairs fail due to patient-related factors and technical-related factors related to the mesh used in the operation. Patient-related factors include scar tissue or a surgical wound from a previous operation that has not healed properly.
- Diabetes: diabetic patients have poor-quality tissue, and the risk of hernia recurrence is high.
- Obesity: being overweight can stretch the abdominal wall and strain the scar tissue, and the chance of repair failing is very high.
- Smokers: In smokers, scar tissue collagen is of inferior quality, and the risk of recurrence is high.
- Heavy lifting: patients who resume heavy lifting very early after hernia surgery can weaken the scar tissue and cause the hernia to come back.
It is more likely to result in infection and failure if the mesh material is extremely thick and has very small pores. Failure can result from mesh that is prone to shrinkage and is too tiny to cover the hernia. It’s possible that some mesh varieties don’t work well at promoting tissue ingrowth. To retain the material in place and provide a sturdy repair, tissue ingrowth is essential.
Causes of Mesh Failure
Infection
When bacteria enter your body, reproduce, and cause illness, an infection results. These pathogens could include bacteria, fungi, viruses, and more. Patients undergoing surgery to treat hernias with mesh frequently get infections. The infection can frequently be treated with medication and rest. Other times, the infection can become fatal, particularly if it has festered or been ignored and manifests years later.
Methicillin-resistant Staphylococcus aureus (MRSA), for example, can spread infection to the mesh and the surrounding environment, rendering the mesh ineffective. Some MRSA-related mesh infections may not show any signs of infection at the wound site; therefore, the patient may not initially recognize that the sickness is due to the mesh implant, but over time, it worsens.
Breakage
When something breaks, it means that it fractures inside the body and some of the mesh product breaks off. The fractured component might then spread an infection or move. The crack has also left the mesh itself with jagged edges. Bowel perforation and blockage have both been linked to the fractured piece and the mesh itself.
Shrinkage
Mesh contraction, often referred to as mesh shrinkage, is the process through which mesh loses some of its initial size. Shrinkage may result in blockage, migration, infection, and chronic pain. Scar tissue may develop around the mesh as it contracts, forming a fibrous mass with nerves. In some cases, the tissue may tear as a result of the shrinkage pulling on it. The mesh product can then move, resulting in more harm.
Migration
Mesh migration happens when the mesh relocates to a different part of the body from where it was placed in the body to treat the hernia. Migration comes in two forms: Migration that is mechanical or primary This migration happens when the mesh is not sufficiently fastened or fixed to the surrounding tissue for it to remain, eventually leading to its movement, typically from an external force.
Secondary Movement. This migration happens when the implant injures the tissue, and to treat it, the body produces granulation to seal the wound. However, the mesh may degrade during the granulation process and then migrate. Months or even years may pass during this procedure. Mesh migrates and causes difficulties in addition to failing to hold the hernia in place and causing complications like chronic pain, infection, serious bleeding, and hernia recurrence.
Rejection
Sometimes during hernia mesh repair surgery, the body will reject the mesh because it views the implant as an invasion and assaults it as a result. The immune system’s assault on the foreign object may manifest as inflammation, which can result in infection and other problems, leading to the failure of the mesh. The immune systems of individuals have been found to react to two particular mesh materials: synthetic materials, such as polypropylene, and animal skin. All mesh products use synthetic or man-made materials, but despite being a known source of problems, polypropylene is still utilized because it is affordable and, when it doesn’t cause issues, performs effectively.
Lack of surgical experience and subpar surgical technique may make mesh failure more likely. Hernias generally have a higher recurrence rate following open surgery than laparoscopic surgery. However, laparoscopic surgery is trickier and requires more training. The best results can only be obtained by accepting a longer learning curve, systematic, well-mentored training, and a high level of standardization of the operational method.
What is the Treatment plan?
In some milder cases, your doctor might advise waiting to treat the hernia before continuing to keep an eye on it. Recurrent hernias can result in extreme pain or discomfort, necessitating elective surgical treatment. Your surgeon might advise elective (non-emergency) surgical repair if that applies to you. In some rare circumstances, urgent or emergency surgery is required. If a recurrent hernia poses a threat of suffocating a section of the intestine, this kind of action will be advised.
A recurring hernia requires surgical closure and reinforcement of the abdominal wall defect, frequently using synthetic mesh material. The procedure your doctor advises will depend on the size and location of your hernia, your general health, and how active you intend to be in the future.